Health
The brain on ketamine

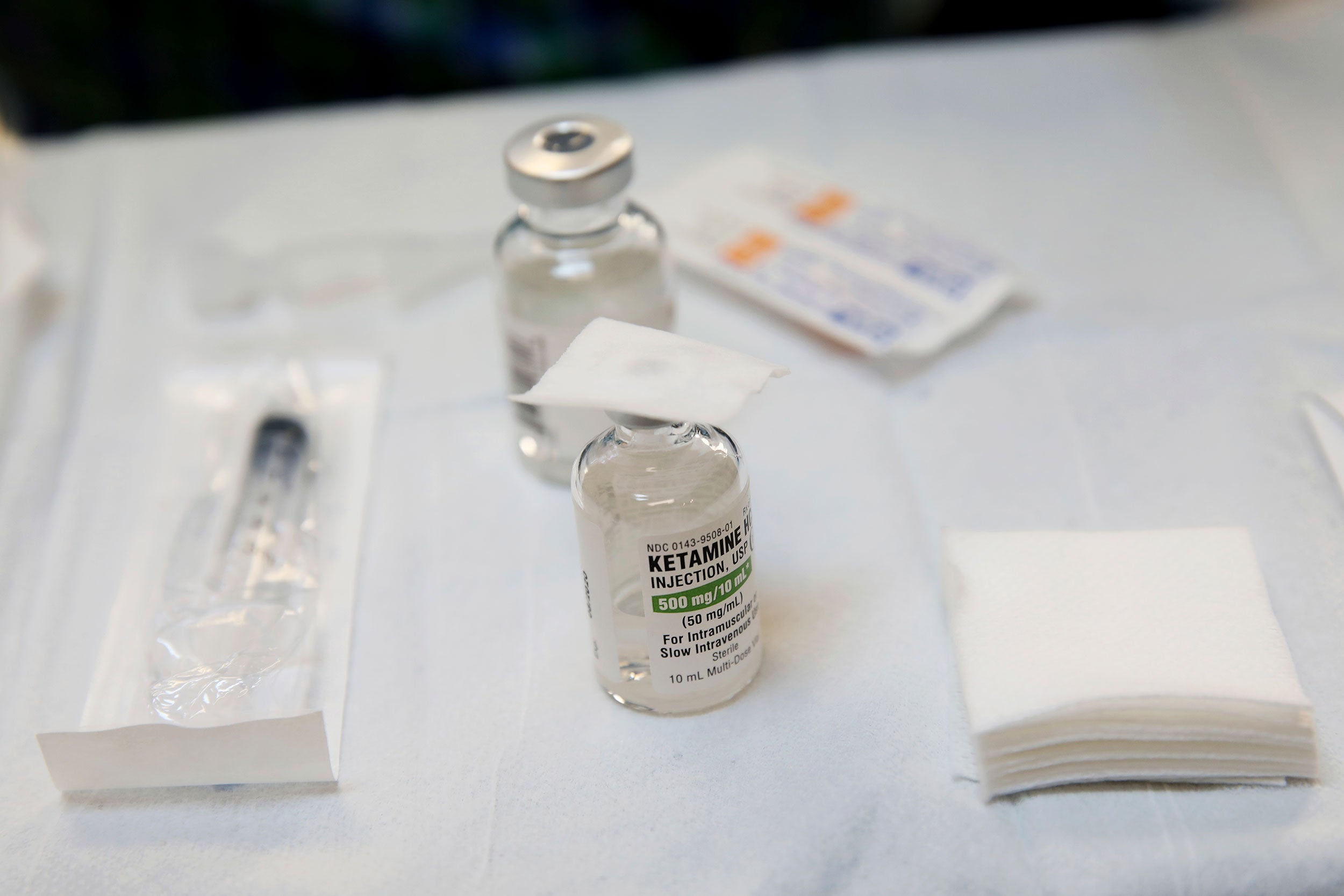
Ketamine was approved by the FDA in 2019 for the treatment of depression, “but its usefulness is limited by its potential for abuse because of its psychiatric side effects,” said Fangyun Tian.
Jon Chase/Harvard Staff Photographer
It’s a powerful antidepressant, but science needs more answers on out-of-body experiences and other ‘dissociative effects’
Deployed as an anesthetic in human and veterinary medicine for decades, the synthetic compound ketamine was approved four years ago as a fast-acting antidepressant. But in addition to its anesthetic and antidepressant potency, the drug has “dissociative effects,” including hallucinations, that have led to recreational use.
Challenges electroconvulsive therapy
Researchers at Massachusetts General Hospital recently traced ketamine’s effects to three brain regions. Two are believed to have a role in the drug’s effectiveness as an antidepressant: the prefrontal cortex — responsible for planning and other executive functions — and the hippocampus, which influences memory formation. The third, the posteromedial cortex, in the back portion of the brain, is a likely site for the dissociative effects.
The Gazette discussed the findings with Fangyun Tian, an instructor in anesthesia at Harvard Medical School and MGH and first author of the paper, which was published in Nature Communications. The interview has been edited for clarity and length.
Q&A
Fangyun Tian
GAZETTE: Ketamine has been around for a long time as anesthesia. What can you tell us about its use for depression?
TIAN: The administration of a subanesthetic dose produces a very rapid and sustained antidepressant effect, comparable to many other traditional antidepressant drugs. It was first approved by the FDA in 2019 for the treatment of depression, but its usefulness is limited by its potential for abuse because of its psychiatric side effects, such as dissociation. So, if we can understand the neurocircuitry mechanisms mediating ketamine’s antidepressant and dissociative effects, that could provide important insights into the development of improved therapies, with fewer side effects and greater safety.
GAZETTE: Though the focus is on treatment of depression, your study was on patients with epilepsy, why?
TIAN: Because they had had electrodes implanted in their brains for a different purpose: to localize their epileptic seizures. They were doing explantation surgery to remove the electrodes, and that gave us a good chance to study EEG [electroencephalogram, which records brain activity] dynamics in cortical and subcortical brain structures. We first took a five-minute baseline recording and then gave the patient ketamine. Then, after a 14-minute infusion period, we asked the patients to answer questions that allowed us to evaluate their dissociative states. After that, the patients were given a general anesthesia for their surgery. We did EEG recordings during the whole process.
In our experiments, we separated the ketamine infusion from the induction of general anesthesia for the surgery, during which a different anesthetic, propofol, was used.
GAZETTE: What did you find?
TIAN: We found gamma oscillations — very-high-frequency oscillations — in the prefrontal cortex and the hippocampus. These are regions that are known to be involved in ketamine’s antidepressant effects from other studies. We also found a three-hertz oscillation in the posteromedial cortex, called the PMC, that another study showed might be related to ketamine’s dissociative effects. So, it seems that different brain regions are involved in ketamine’s antidepressant and dissociative effects. It might be possible to develop future therapeutics that can avoid dissociation.
GAZETTE: How do patients experience these dissociative effects?
TIAN: They feel that they are disconnected from their feelings, thoughts, surroundings, and identity. We used a questionnaire called the Clinician-Administered Dissociative States Scale, or CADSS, to evaluate the dissociative state. We ask questions like, “Do things seem to be unreal to you, as if you were in a dream?” Or: “Do colors seem to be diminished in intensity?” The answers varied among patients, but most answered “yes” to a large proportion of these questions. The dissociative effects are pretty prevalent in patients taking ketamine.
GAZETTE: Is it pronounced enough that people with depression who might benefit don’t want to take the drug?
TIAN: It might be one of the reasons. It’s more severe in some patients but less in others. It depends on the person.
GAZETTE: Is this effect also the reason it’s used recreationally?
TIAN: Yes. It could cause hallucinations, make things seem unreal, or produce an out-of-body experience.
GAZETTE: What is next for you in this research?
TIAN: I want to do a follow-up study in patients with treatment-resistant depression to see if the brain rhythms we found in this study correlate distinctly with antidepressant and dissociative effects which may vary between patients.
GAZETTE: How did you get interested in this research?
TIAN: As researchers in the Department of Anesthesia we are very interested in the mechanisms of how anesthetic drugs work so that we can provide better care for patients. We are interested in identifying biomarkers that allow us to measure brain states clinically, and particularly in finding biomarkers for unconsciousness. The primary tool we use to measure brain states is the EEG. We found that different anesthetic drugs, like propofol, ketamine, sevoflurane, and dexmedetomidine, cause very distinct brain oscillatory patterns. Ketamine is the only one that induces the high-frequency gamma oscillations. At high doses, ketamine can induce general anesthesia — unconsciousness — but at low doses, it causes these antidepressant and dissociative effects. It’s a very unique and very important drug. We want to know what happens at the molecular level and at the neural circuit level that could cause these different effects.